Updated August 3, 2022

Do you know how to calculate your due date? Establishing an accurate due date, also known as your estimated date of confinement or EDC, is extremely important.
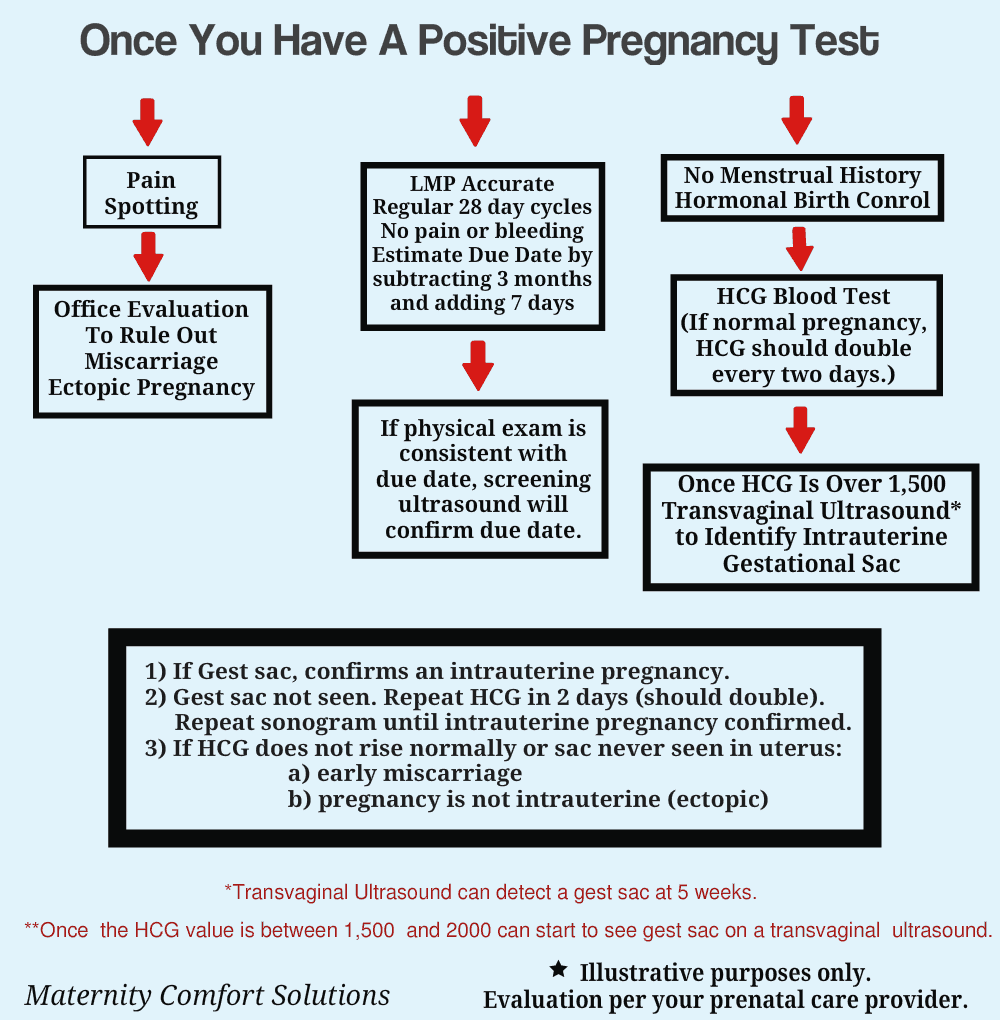
If the first day of your last menstrual period is accurate, you can calculate your due date by subtracting three months and adding seven days to the first day of your last menstrual period.
You may need more testing to confirm an accurate due date if:
- You are not sure about the first day of your last menstrual period.
- Your menstrual cycle is not a regular 28-day cycle.
- If the number of weeks pregnant based on your physical exam is not consistent with your due date based on your LMP.
Why is it so important to establish an accurate due date?
Your provider will want to establish an accurate due date as early in your pregnancy as possible. Your estimated date of confinement* will impact the timing and accuracy of many medical tests. It will also affect many medical decisions throughout your pregnancy.
* Estimated date of confinement is the clinical term used to define your due date. It is often referred to as your EDC.

The following is a list of tests and medical decisions that can be affected based on your EDC:
- Screening Blood Tests
- Management Decisions About Premature labor
- Medical Decisions If You Go Past Your Due Date
- Fetal Growth Measurements
- Decisions About When To Deliver If There Are Pregnancy Complications
How To Calculate Your Due Date (Estimated Date of Confinement)
To calculate your estimated date of confinement (EDC), you will be asked detailed information about your menstrual cycle.
If the decision is made to use your due date based on your LMP, your provider will want to know the first day of your last menstrual period and will want to know that you are certain about this date.
The “menstrual date” will permanently be entered into your prenatal record and will not be changed.
Example: If you are 10 weeks pregnant based on your LMP and your exam at your first prenatal visit indicates you are 16 weeks, an ultrasound will be performed to determine your due date. This is because there is too large a discrepancy between your due date based on your menstrual cycle compared to your clinical exam.
What questions will I be asked about my menstrual cycle?
1) What was the first day of your last menstrual period (LMP)?
This determines when you ovulated if you have a regular, 28-day menstrual cycle. During ovulation, the egg is released from the ovarian follicle.
Here are some useful facts about your menstrual cycle:
- A 28-day menstrual cycle is divided into a proliferative phase (the 1st 14 days) and a luteal phase (the last 14 days).
- During the proliferative phase (also known as the follicular phase), ovarian follicles in the ovary start to mature. Each follicle has an egg. Ultimately, one follicle will be chosen to release an egg during ovulation on day 14.
- During the proliferative phase, the menstrual lining is being hormonally prepared for implantation.
- The luteal phase starts with ovulation (Day 14) and ends with the first day of your next period (unless pregnancy occurs).
- If the egg is fertilized in the fallopian tube it will be transported into the uterine cavity to implant on the uterine wall.
2. Are you sure about the first day of your last menstrual period (LMP)?
You want to be sure because this date will be used to calculate your due date.
3. What was the first day of your previous menstrual cycle?
This helps to determine if your menstrual cycle is reliable for calculating your due date.
4. Did your last period (menstrual cycle) start on the right day and last the normal number of days?
Again, this can help determine the accuracy of your LMP.
5. What is the usual number of days between your periods (from Day 1 to Day 1)?
This helps to determine how reliable your period is for determining your due date. If you have very consistent 28 day periods that you have regular midcycle ovulation.
6. At what age did you start having periods?
Menses can be irregular when they start (menarche) and when they end (menopause). This information can also help to determine how accurate your last menstrual period is.
7. Did you take any home pregnancy tests before this visit? If so, what date did you first get a positive test?
If accurate, it is the best indicator of when you first documented you were pregnant.
8. Do you know the day you got pregnant?
Fertilization can happen for a few days after intercourse.
10. Do you have a history of infertility due to irregular periods?
Infertility is often associated with irregular periods, delayed ovulation, and anovulation (not ovulating). If you conceived without infertility treatment, this information can be helpful.
11. Were you taking the birth control pill or another form of hormonal contraception when you got pregnant?
- Hormonal birth control can interfere with your period and this can make your last menstrual period unreliable.
- If your menstrual cycle is not reliable, it may be necessary to use blood tests (HCG) and ultrasound to calculate your due date.
- Once your due date is determined early in your pregnancy, it will not change since there will be no tests for dating that will be more accurate. As noted below, ultrasound evaluation for determining your due date gets less accurate as your pregnancy advances.
How is ultrasound used to calculate your estimated date of confinement?
First Trimester:
An ultrasound performed under 12 weeks of pregnancy will give the most accurate information to calculate your due date. This is because the ultrasonographer can see changes over a short period of time.
In contrast, an ultrasound done during the third trimester of pregnancy is very inaccurate because the fetus is fully developed and changes in imaging are very subtle.
The reason first-trimester ultrasound so accurate to calculate your due date is because distinct ultrasound findings occur every few days.
These findings can be accurate to within 5 days, depending on:
- The quality of equipment used
- The experience of the sonographer
- Whether the ultrasound is transvaginal or transabdominal. (Almost all early ultrasounds are now done transvaginally.)
The specific findings on a 1st-trimester ultrasound are listed below. They offer information about dating and fetal well-being:
-
Gestational Sac:
The gestational sac can be seen as early as the 4th week of pregnancy. However, it is not uncommon to become visible between the 5th and 6th week.
This is the earliest finding to confirm that the pregnancy is developing in the uterus. Often times this ultrasound finding is compared to a blood test called an HCG (Human Chorionic Gonadotropin).
It has been determined that when this blood test is above 2500 an intrauterine sac should be visible.
If not there may be no problem because the laboratory measurement can vary and if one has twins the levels of HCG will be higher.
The most important reason your provider will want to confirm an intrauterine pregnancy once your HCG reaches 2500 is to exclude the possibility of having an extrauterine pregnancy.
This is a pregnancy that is developing but is not implanted in the uterine cavity. Pregnancies that implant outside the uterine cavity are called ectopic pregnancies. Most often ectopic pregnancies are located in the fallopian tube.
It is very important to diagnose an ectopic pregnancy as soon as possible so treatment can be initiated before the pregnancy enlarges and ruptures out of the tube.
This can lead to significant blood loss and even death if not diagnosed and managed properly.
-
Fetal Heart Rate:
Ultrasound detection of a fetal heartbeat can be detected as early as 5 1/2 weeks. However, it is not uncommon to not see a heartbeat before 6 or even 7 weeks.
The reasons for this are many including some that have been mentioned.
-
Yolk sac and Fetal Pole:
This finding of a yolk sac confirms the presence of a developing embryo within the gestational sac. The yolk sac supplies nutrition to the developing embryo until nutrition is supplied by the placenta.
Visualization of a fetal pole with a heartbeat confirms the development of a viable developing embryo.
A yolk sac and fetal pole can start to be seen with a transvaginal ultrasound around 5 1/2 to 6 1/2 weeks.
-
Crown-Rump length:
When your pregnancy advances to 7 to 12 weeks, ultrasound dating is no longer based on the gestational sac, fetal pole or yolk sac. At this stage during your pregnancy, the crown-rump length is the ultrasound measurement used to calculate your due date.
Second Trimester
If you have a second-trimester ultrasound, it will be less accurate than a first-trimester ultrasound.
This is because second-trimester ultrasound changes from one week to the next are very subtle compared to the dramatic changes that occur in the first trimester.
During the second trimester, an ultrasound performed to establish a due date measures the fetal head diameter (Biparietal Diameter) and other fetal growth characteristics. The accuracy of these fetal growth parameters is only accurate to within 11 days.
* The accuracy of an ultrasound study also depends on the experience of the sonographer and the quality of the equipment.
Third Trimester
For the same reasons noted above a third-trimester ultrasound is less accurate and can have a margin of error of up to three weeks. Changes in fetal development from one week to the next are very subtle in the third trimester. This is the reason the due date will not be accurate.
This being said, a third-trimester ultrasound will be the only dating option available if you have your first prenatal appointment in the third trimester and your due date is not consistent with your last menstrual period.
How to calculate your due date based on your menstrual cycle:
If you have a regular 28-day menstrual cycle, there is a simple formula to get a quick idea of when your due date will be. Make sure you confirm your due date with your health care provider.
Subtract 3 months from the 1st day of your last menstrual period and add 7 days. (Source)
*This formula assumes you have ovulatory, regular 28-day cycles.
How your provider will calculate your due date?
Information used to calculate your estimated date of confinement (EDC):
- Last Menstrual Period – The first day of your last menstrual period.
- Pregnancy Test Hormone: HGC (quantitative measurement) – This test measures the level of human chorionic gonadotropin (HCG). It is used to determine if you are pregnant and if the pregnancy is
- First Trimester Ultrasound
Conclusion:
- Your prenatal care provider will determine your due date based on the information you provide at your first prenatal visit.
- Testing (blood tests, ultrasound) will be used to determine your due date if the first day of your LMP is not accurate.
Other articles you may find helpful:
- 10 Must-know Tips for Your First Prenatal Visit
- 9 Questions You Must Ask At Your First Prenatal Visit
- 10 First Trimester Pregnancy Tips You’ll Be Glad to Know
Common Questions About Calculating Your Due Date (EDC):
How do you calculate your due date?
Assuming your last menstrual period is accurate, there are two simple formulas using the first day of your last menstrual period:
- Subtract 3 months and add 7 days to the first day of your last menstrual period.
- Add 280 days to the first day of your last menstrual period.
How can you determine when you conceived based on your due date?
If your menstrual cycle is 28 days and your due date was calculated by your provider based on your last menstrual period, conception occurred around day 14 of your last menstrual period.