Updated October 25, 2023
“Your first prenatal visit is a blend of understanding and celebration. It’s where we gather insights about your health, establish a foundation for the journey ahead, and most importantly, ensure that both you and your baby are on a path to wellness. Remember, every question is valid, every emotion is understood, and you’re never alone in this journey. We’re here to support, guide, and cherish these moments with you.” – Dr. Doug Penta, MD, OB/GYN
These 9 questions are based on our 25 years of clinical experience managing prenatal patients from their first prenatal visit until delivery.
The following list is simply a list of the questions from this article and is only a few of the many questions you may have for your healthcare provider.
Write the questions down as you will surely have questions specific to your medical history.
- Who will deliver my baby when I go into labor?
- If I require urgent care, where will I be seen, and who will evaluate me if my provider is not available?
- Do the providers in your practice manage labor from home or is there always one provider present at the hospital?
- How is anesthesia coverage managed at the hospital affiliated with your medical practice?
- At my prenatal visit, can I book more than one appointment at a time so I can see my personal prenatal care provider?
- How do you manage patients with an overdue pregnancy?
- What is the level of nursery at the hospital affiliated with your practice?
- How do the providers in your practice feel about pain control during labor and delivery?
- What childbirth preparation classes do you recommend to your patients?

The questions are intended to be topics that will help educate and initiate a conversation with your prenatal care provider and are not all-inclusive.
There are many other very important questions you will have, based on your particular desires and expectations.
Asking these questions at the start of your prenatal care is very important.
You want to know if your prenatal care provider has any fundamental differences in beliefs or expectations about your prenatal care, labor, and delivery.
It will be comforting to know the answers to these questions as your pregnancy advances.

(Couple at a prenatal visit.)
9 Questions You Must Ask At Your First Prenatal Visit
1. Who will deliver my baby when I go into labor?
Every women’s health medical practice caring for prenatal patients has a labor and delivery schedule arranged months in advance.
This schedule indicates what medical group provider, will be managing labor patients in labor and delivery 24/7/365.
This schedule is usually made 3 to 6 months in advance, to avoid any scheduling conflicts.
There are also medical practices that have doctors who only cover patients in labor and delivery.
These physicians are called laborists.
This role was created to improve the continuity of care for patients in the hospital.
When you go into labor, you will be managed by the doctor covering labor and delivery based on the call schedule discussed above.
It is not physically possible nor safe for one doctor to cover labor and delivery 24 hours a day, every day.
There are a few clinical situations where you would be more likely to be delivered by your doctor:
- If you are having an induction, your doctor may schedule it when on call at the hospital.
- Scheduled repeat cesarean section. (If you know at your first prenatal appointment that you are going to want a repeat cesarean section, discuss this at your first visit.)
2. If I require urgent care during my pregnancy, where will I be seen, and who will evaluate me if my provider is not available?
The answer to this question differs a great deal from one medical practice to another.
Before you choose a provider, you will want to find out how the medical practice cares for patients when the office is closed and what facilities (if any) are available when it comes to managing problems after office hours.
Questions that will help determine who will manage your care after hours are the following:
- What is the size of the medical practice? How many doctors in the medical group?
- Do the group of physicians in the medical practice manage labor and delivery at one hospital?
- Is the practice part of a larger network of physicians who manage patients at more than one hospital?
- Does the medical practice have an urgent-care facility to evaluate labor patients before sending patients to the hospital? A medical practice such as Kaiser Permanente has urgent care facilities to evaluate patients after office hours.
- How many doctors in the medical practice manage labor patients in the hospital?
Once you know the answers to the questions above, you will have a far better idea of how you will be managed for non-scheduled medical visits.
Since you may be managed by another doctor in your medical group, it is a good idea to schedule a prenatal visit with each of the doctors in the practice that may cover your labor and delivery. This will ensure that you will have at least meet the doctor delivering your baby before the onset of labor. -Dr. Doug Penta, MD
3. Do the providers in your practice manage labor from home or is there always one provider present at the hospital?
There are very few medical practices that cover labor and delivery from home. This was not uncommon years ago.
However, now that most medical practices have three or more doctors, more patients are managed by one medical practice. This means there will be more patients in labor at any given time.
Some medical practices and hospitals now employ laborists.
These doctors only cover patients in labor and delivery.
4. How is anesthesia coverage managed at the hospital affiliated with your medical practice?
- It is important to know how the anesthesia department covers patients in labor at the facility where you plan to deliver.
- This is important to know even if you are not planning on using pain medication during labor.
- Should you need urgent intervention during your labor, anesthesia will be necessary
- Anesthesiologists are employed by the hospital. The way the anesthesia staff cover labor and delivery will vary depending on the hospital where you plan to deliver.
- A level one hospital will have a different coverage arrangement compared to a tertiary care hospital that has 24/7 in-house anesthesia coverage at all times. Tertiary care hospitals are most often teaching hospitals and trauma centers. Most often they have to have a full complement of medical staff in the hospital at all times.
- This means from medical students to residents to attending physicians to fellows, these hospitals have a full obstetric anesthesia staff as illustrated in our article on 20 hospital questions.
5. At my prenatal visit, can I book more than one appointment at a time so I can see my personal prenatal care provider?
Many women want to schedule more than one prenatal visit at a time to get an appointment time that fits into their work schedule and is with their personal provider.
Though many offices will book appointments far out, some will not.
Take the time to ask this question if you feel this will impact your daily routine.
Especially since there are many routine prenatal visits during your pregnancy.
6. How do you manage patients with an overdue pregnancy?
Doctors and patients often have a difference in opinion about how to manage a pregnancy that goes past the due date.

First, it is important to mention the terms that are used to describe this situation.
Most people will use the terms “overdue pregnancy” or a “pregnancy that has gone past the due date”.
In the medical field, the term used to describe a past-due pregnancy depends on how many days over the due date.
Making this distinction is important because it will determine what management is necessary:
Late-term pregnancy: 41 – 41 6/7 weeks
Post-term pregnancy: 42 weeks and beyond
There are basically two approaches to the management of pregnancies that do not deliver by 41 weeks:
1. Induction:
Inducing labor is based on a number of clinical criteria.
This intervention can be done electively to prevent complications associated with a late-term or post-term pregnancy.
Inducing labor is also done immediately (non-electively) if delivery is necessary because of a pregnancy complication or abnormal fetal testing during expectant management (#2)
2. Expectant management:
Expectant management involves the clinical observation and monitoring of a late-term pregnancy until the onset of spontaneous labor.
Monitoring includes antenatal testing (fetal testing) to monitor fetal well-being. (The problem with this approach is that antenatal testing is not 100% reliable when it comes to assessing fetal well-being.)
In either situation, the decision to proceed with the induction of labor is done if there are concerns about infant morbidity and mortality or maternal concerns of morbidity and mortality.
Assuming a pregnancy is uncomplicated there is no disagreement about allowing a pregnancy to go one week past its due date or to 41 weeks gestation.
In fact, the majority of pregnancies will deliver within one week before or after the scheduled due date.
At 41 completed weeks of pregnancy is when decisions about delivery are made.
Balancing the risk of induction versus the risk of fetal morbidity or mortality.
- It has been well established that the function of the placenta starts to deteriorate during the weeks following delivery. A term used to describe this process is uteroplacental insufficiency. When this happens there can be decreased blood flow and oxygen delivery to the fetus.
Induction of labor will be decided upon by your provider based on a number of factors and options that are within the standard of medical care:
- Inducibility of cervix: A cervix that is inducible based on a cervical exam can lead to more successful induction of labor.
- Maternal health conditions: high blood pressure (toxemia, etc.)
- Completed weeks of pregnancy
- Fetal testing findings
- Provider’s preferred management approach (assuming there are options).
Management decisions cannot be generalized as there are a number of factors (above) that need to be considered to determine the best treatment option.
*Complying with the accepted standards of medical care is the one factor that must be part of any plan of management.
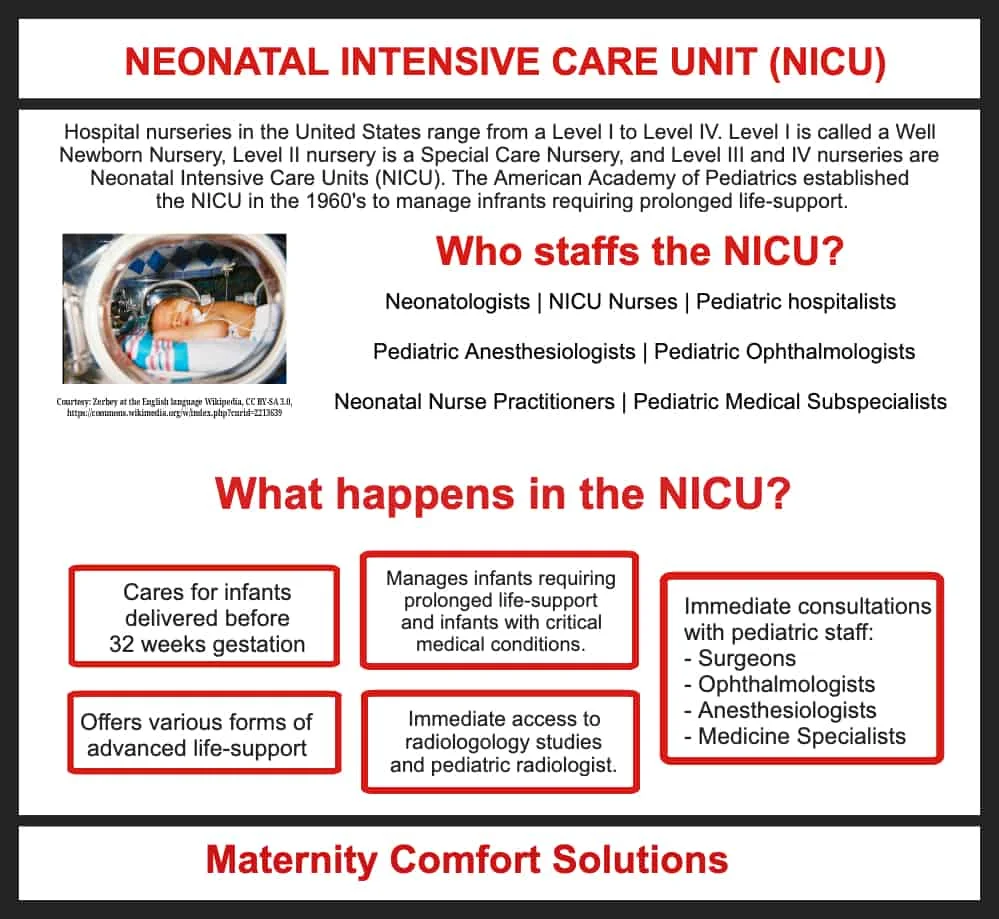
7. What is the level of nursery at the hospital affiliated with your practice?

Knowing the level of nursery at the hospital where you plan to deliver is extremely important.
The care can range from a Level I (Well Baby Nursery) to a Level II (Special Care Nursery) to a Level III or Neonatal intensive care unit (NICU).
The NICU was first established in the 1960s by the American Academy of Pediatrics to manage babies with critical medical problems requiring prolonged life support.
The level of the nursery essentially correlates with the level of the hospital. Hospitals range from primary to secondary to tertiary care facilities.
Typically, tertiary care hospitals are teaching hospitals and are equipped to handle trauma and advanced medical care.
If you have a medical illness or a pregnancy-related complication that could affect the health of your baby, it is important to know what level of neonatal care is available at the hospital where you deliver.
8. How do the providers in your practice feel about pain control during labor and delivery?

Many women choose a doctor for their pregnancy based on a mutual understanding and agreement on pain management during labor.
The choices for pain control during labor cover a broad spectrum:
- Strongly desiring to go through natural childbirth without the use of medication during labor.
- Want an epidural for pain management as soon as it can be administered? When an epidural can be administered is based on criteria that have been defined and comply with the standards of medical care.
- For women who are not sure if they will want IV pain medication or an epidural, the decision can be managed during labor. It is not a problem to change your mind about pain management, as long as there is adequate time to administer alternative therapies. You do not want to delay your decision too long. Epidurals take time to administer, so it is important to decide well before you are fully dilated and imminently going to deliver.
When deciding on pain control during labor, it is very important to plan ahead as best you can.
Most importantly, be prepared to accept the possibility that your pain management during labor might deviate from your birth plan.
The two most common reasons are a personal desire for pain control and the need for regional anesthesia (spinal or epidural) if a cesarean section is necessary.
Some of the clinical guidelines that have to be met before epidural placement include:
- Confirmation that you are in labor, best defined as contractions with cervical change.
- Cervical dilatation … which you will want to discuss with your provider. Some medical practitioners and medical facilities are fine with giving an epidural as long as you are in labor, even if you are in early (latent) labor. Other doctors may want to wait until cervical dilatation has reached 3 cm.
- No history of medical conditions that could interfere with the safe placement of an epidural catheter. Two such conditions include bleeding disorders or a history of severe back injuries.
The doctors in a medical group share hospital coverage to manage patients in labor.
Try to arrange prenatal visits with the other doctors so you can ask questions and know that they are in agreement with your labor plan.
Solo practitioners who managed everything during your prenatal care and delivery (with rare exceptions) no longer exist.
This is a result of the advances that have been made in the management of pregnancy, the costly overhead of running a practice, and the number of patients that have been determined to be safe for one practitioner to care for.
This is why it is crucial to know the questions you must ask at the first prenatal visit.
So you will want to discuss your philosophy and wishes about pain control.
Be sure to ask questions. There is a lot of misinformation that circulates online.

(Woman with an epidural self-administering a dose of pain medication.)
While you certainly don’t need to have any type of birth plan thought out at your first prenatal visit, it isn’t a bad idea to at least consider how you see your future labor and delivery experience unfolding.
You can check out our post on developing a stress-free birth plan for some questions you might want to consider about the birth process.
9. What childbirth preparation classes do you recommend to your patients?
Many couples have specific requests when it comes to their pregnancy and birth plans.
It is not unusual for expectant parents and their prenatal care providers to disagree on management options.
This is often the result of a difference in philosophies or expectations about the childbirth experience. What is most important is that the management that is agreed upon is within the standards of medical care.
This question is addressed in detail in our post Are Childbirth Classes Necessary?
Other pregnancy-related articles you may find helpful are the following:
- 5 Must-Know Tips For Scheduling Prenatal Visits
- 10 Tips To Fight Fatigue During Pregnancy
- Maternity Hospital Tour: 20 Important Questions You Should Ask
FAQ’s
1. Should my husband come to my first prenatal visit?
Dr. Doug Penta, MD, OB/GYN with over 38 years of experience and a father of two: “Absolutely, if he can and if you both feel comfortable with it. The first prenatal visit is a milestone, and having your partner there can be a great support. Not only will he get firsthand information about the pregnancy, but it also provides an opportunity for him to ask questions, understand the process, and be an active participant from the get-go. It can foster a feeling of shared responsibility and excitement about the journey ahead.”
Sue Winters, RN, and mom who had her husband attend her first prenatal visit: “For us, having my husband there was a game-changer. It made the experience feel even more real and shared. He was able to ask questions that I hadn’t thought of, and it was reassuring for both of us to hear the answers together. Plus, there’s something so special about experiencing those initial moments as a team. It truly set the tone for our pregnancy.”
2. What blood tests were done at my first prenatal appointment?
The initial panel of blood work, done at your first prenatal has been evolving over many years.
Testing will continue to evolve, as tests are identified that can help to screen for medical and developmental concerns during pregnancy.
As of this moment, a typical blood work screen at your initial prenatal visit will include the following:
- Blood Type and Rh Factor (ABO blood group and if Rh + or -). Even if you know your blood type you will still be checked for a number of medical reasons.
- Hepatitis B Screening
- Rubella Screening
- VDRL (Syphyllis screening)
- Thyroid Screening (This is a newer addition to the bloodwork panel because of the impact undiagnosed under or over-thyroid activity can have on fetal development.
- HIV screening if consented to.
- Genetic testing depends on a risk profile such as an inherited condition or ethnic-related genetic disorder.
- Blood count
- Metabolic panel
- Urine test for routine urinalysis
What happens at your first prenatal visit?
According to Dr. Douglas Penta, MD, your first prenatal visit is a significant step in your pregnancy journey. It’s an opportunity to establish a health baseline, get answers to any questions, and set the tone for your prenatal care.
Here’s a breakdown of what typically happens:
- Medical History Review: Your healthcare provider will ask about your personal and family medical history, including previous pregnancies, surgeries, medications, and any chronic conditions. This helps identify potential risk factors or concerns.
- Physical Examination: This includes checking your weight, blood pressure, heart, lungs, and sometimes a breast and pelvic exam. The pelvic exam allows the doctor to determine the size of your uterus and may also include a Pap smear if you’re due for one.
- Calculation of Due Date: Based on the first day of your last menstrual period (LMP) and sometimes supplemented by ultrasound, your provider will estimate your due date.
- Blood and Urine Tests: These tests can:
- Determine your blood type and Rh factor.
- Check for anemia.
- Screen for infections such as rubella, syphilis, hepatitis B, HIV, and others.
- Check for immunity to certain diseases.
- Screen for urinary tract infections or kidney problems.
- Discussion of Lifestyle Habits: Expect to discuss topics like nutrition, exercise, medications, and any potential harmful habits like smoking, alcohol, or drug use.
- Ultrasound: Some healthcare providers might conduct an ultrasound during the first visit, especially if there are uncertainties about the pregnancy timeline or concerns about the pregnancy.
- Prenatal Vitamins: If you’re not already on prenatal vitamins, your provider will likely recommend starting them. These vitamins contain essential nutrients, including folic acid, which is crucial during early pregnancy.
- Questions and Concerns: Your provider should allocate time to answer any questions or concerns you might have, whether they’re about symptoms, what’s to come, birthing plans, or anything else on your mind.
- Scheduling Future Appointments: Your next prenatal visits will be discussed, and you’ll likely leave with a schedule or an idea of how often you should be seen.
- Counseling: Depending on your medical history, age, or other factors, you might be offered genetic counseling or screening tests to assess the risk of genetic disorders
Make sure you address any questions or concerns you have about COVID-19.
The information about coronavirus testing and how it is managed during pregnancy is constantly being updated as data becomes available from the CDC.